University of Surrey Researchers Develop AI Model to Predict Knee X-rays One Year Ahead Transforming Osteoarthritis Care
University of Surrey researchers have developed an AI model that predicts what a patient’s knee X-ray will look like a year in the future, providing a visual forecast and risk score for osteoarthritis progression and promising breakthroughs in AI-assisted healthcare diagnostics.
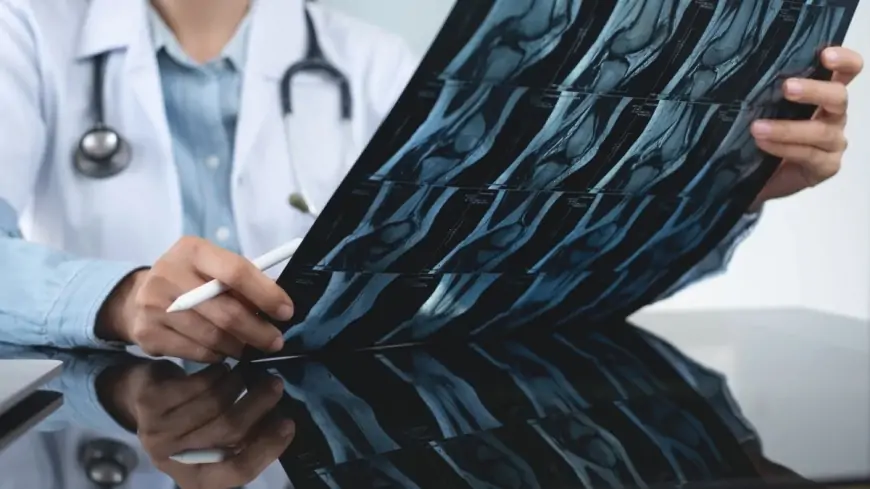
Researchers at the University of Surrey have developed a groundbreaking AI model capable of predicting a patient’s knee X-ray image one year into the future. This innovative technology represents a breakthrough in AI-assisted healthcare diagnostics, particularly for osteoarthritis, a degenerative joint condition affecting over 500 million people globally and a leading cause of disability among older adults.
Presented at the International Conference on Medical Image Computing and Computer Assisted Intervention (MICCAI 2025), the AI system uses a sophisticated generative diffusion model trained on nearly 50,000 knee X-rays from roughly 5,000 patients. It not only generates a realistic “future” X-ray image but also provides a personalized risk score that estimates disease progression. This dual output equips doctors and patients with a visual roadmap to anticipate changes and tailor treatment plans proactively.
David Butler, the study’s lead author from the University of Surrey’s Centre for Vision, Speech and Signal Processing, explained that their system bridges a critical communication gap in medical AI. Unlike traditional tools that offer only numerical risk predictions, their method visually compares current and projected knee conditions side by side. This visualization serves as a powerful motivator for patients to adhere to treatment regimens or lifestyle changes, while giving clinicians clearer insights that enable earlier intervention.
The AI model identifies 16 key anatomical points within the joint to highlight areas most at risk, enhancing transparency and clinician confidence in the tool’s recommendations. Compared to earlier prediction models, this system operates roughly nine times faster and is more compact, making it practical for real-world clinical integration.
Researchers believe this breakthrough could soon be adapted to predict progression in other chronic conditions like lung and heart diseases, offering similar visual and prognostic benefits. The Surrey team is actively seeking partnerships to deploy this AI innovation into routine healthcare, potentially transforming how millions of osteoarthritis patients manage their health and improving outcomes.
This advance underscores how AI is redefining medical diagnostics by combining accuracy, explainability, and actionable insights to support personalized, preventative care.